Obstetric Brachial Plexus Palsy (Erb’s Palsy)
Birth brachial plexus palsies (obstetric Brachial Plexus Plays, OBPP or Erb’s Palsy)
If you have come here to find out more about obstetric brachial plexus palsy (often called Erb’s palsy) then please read the information below. It is no substitute for a consultation and I am sure will prompt as many questions as answers.
Background
Wilhelm Heinrich Erb was a Bavarian nerve doctor working in the later 19th Century. He gave his name to an injury of the nerves of the brachial plexus which happens at the time of birth: Erb’s Palsy. The word palsy means weakness and the problem described by Erb was a weakness of the muscles of the shoulder and elbow from an injury the child sustained during birth.
There is much we have learnt about this injury since then and still very much to learn.
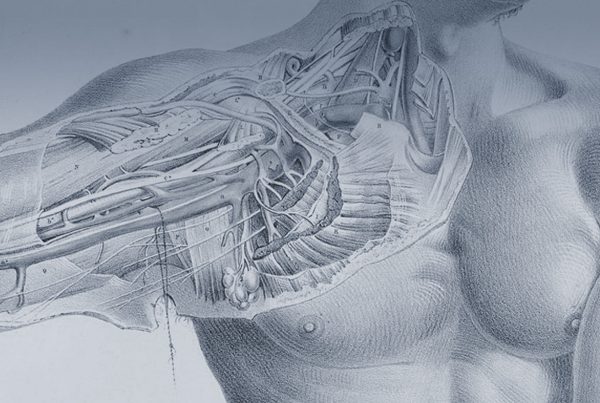
The nerves of the arm leave the spine at five levels (like floors of a building) they are called C5, C6, C7, C8 and T1. These nerve ‘roots’ are made up of hundreds of thousands of nerve cells which then all intermingle at a major junction called the brachial plexus. The injury of a birth plexus palsy is one of the stretching forces of the delivery, as the child squeezes out of the mother’s pelvis the head can be stretched from the neck pulling on the nerves. Nerves can cope with some stretch but too much damages them. The damage can be quite mild (conduction block) which can revcover completely and quite quickly, or be partially or completely snapped into (rupture) or pulled clean from the spinal cord (avulsion)
I treat obstetric palsy by first making sure I have a full grasp of the type, severity and signs of recovery in your child’s specific case. This involves a number of clinical assessments (best to have the first of these at or before your child is 3 months old). Assessing the injury in Obstetric brachial plexus palsy is not an exact science and there are very few absolutes to work from. For this reason I favour a number of examinations over time (so see and record internal change in the function of the muscles of the arm) and a full neurophysiologic assessment. I will arrange this test for your at Great Ormond Street Hospital with Dr Matthew Pitt, one of the few true international experts in this field. This study, in conjunction with the clinical examinations provides me with a picture of what is likely to happen if we do nothing at all- The natural history. It is from this point of understand the natural history that we can determine if any intervention (surgery) can improve upon this. If I think surgery can offer a benefit then we can discuss what this might mean for you and your child- see here. I will never force or carol any one into surgery, certainly not when it is your child that we are all trying to agree the best way forward. I will offer my opinion and discuss your questions, leaving you time to agree between you and those you turn to for help with these difficult decisions.
The nerve injury in OBPP
The stretch injury to the nerves in OBPP is a very different injury to an adult brachial plexus injury. The nerves at this age are much more compliant and stretchy, the injury force is much less and applied much more slowly than it is in a standard road traffic accident. Due to these and other factors the nerve injury in OBPP almost always a neuroma in continuity. This means far from being torn into two pieces the nerve has been damaged but not all the cells injured completely and many of those are capable of regrowing across the area of injury. There are some cases where this is is not the case; it can be that the nerves are so badly damaged that the injured area will not likely recover and it is these cases that require the injured area to be cut out and new channels (nerve graft) to be laid in the gap.
In order to work out if surgery to cut out the damaged part of the nerve is necessary it is important to use every useful assessment we have. We thus use clinical examination along side neurophysiology to make this assessment. Neurophysiology is medical circuit testing, just like the electrician might do at your home. We call on the opinion of a very highly skilled neurophysiologist (a Doctor who specialises in this circuit testing) at Great Ormond Street; Dr Matthew Pitt. He is able to provide information not just on the likely condition of the nerves but also on the state of recovery and the connections of the nerves to the muscles in the arm. This information we have used to classify OBPP into different groups (for each of the 5 nerve roots).
Simply put, the first group is those that will have a great outcome
The next group is those that will do pretty well (not perfectly but ok) but in whom we do not think we can improve things through primary nerve surgery (cutting out the neuroma in continuity and reconstructing the defect with nerve grafts)
The third group is one where surgery is likely to improve the outcome.
There are many options to improve the outcome in OBPP. The first to discuss is Primary nerve surgery.
Summary
This is an operation on the nerves of the brachial plexus in the neck, it is termed an exploration and neurolysis, intra-operative neurophysiologic assessment and proceed to graft and or nerve transfers. This is quite a mouthful- let me explain what it means: The most important point is that the operation should be looked upon as a test, the first part of the operation is to get more information about the kind of nerve injury that your child has. Then, if it appears that cutting out the damaged segments of nerve or re-routing some nerves will improve the situation then I will continue on to do that part of the operation as well.
If I think this operation will improve your child’s outcome and you agree that you want your child to undergo the surgery I will arrange the operation. The operation involves a cut in the neck just above the collar bone (this is a very cosmetic scar and is almost not noticeable when the child grows up). The operation is then to find the nerves of the brachial plexus and free them from the scar tissue which forms after the nerves are damaged. Then I again retest the nerves – just like the test performed before surgery. This is to be very sure that we use all the available and most unto date information before cutting any of your child’s nerves. If there are signs that the nerves are recovering well on their own and that we have released the nerves from scar it might be I go no further and sew up the wound. In other cases the damage is so bad that I might have to take nerves from your child’s leg and splice then into the brachial plexus or reroute some other, undamaged nerves from near by.
The most important feature to understand about nerve surgery, particularly nerve grafting and nerve transfers, is that it is not like rewiring a light bulb- but more like turning on a tap attache to a hose pipe. There is no sudden change, The situation after the operation is often no different in terms of the movements possible than before surgery. Surgery has allowed recovery to take place not actually fixed the nerves directly. Thus just like turning a tap on attached to a hose pipe, things take time to recover, the water has to flow down the whole length of the hose before any water is seen: In nerve surgery this means the regeneration often shows no sign of improvement for many months and full improvement not for a number of years after surgery. A bit like turning an oil tanker (i am told by someone who knows ) it takes time, surgery is like turning the ships wheel but you don’t see the change for a long time.
Further information
The surgery is not a small thing and is not something that we would undertake unless we thought there would be a clear benefit from surgery. If the chances of improving the outcome are low then the risks (which i will come to in a moment) would not be worth it. Therefore it is important that as far as possible we make the correct decision, many in the world rely just on clinical examination then never test the nerves and go a head without all the information to cut out an neuroma in continuity which could have recovered as well or better if it had been left alone. I don’t think that is a good idea and see the act of cutting out the neuroma in continuity as something that should only be performed if we are sure it will improve the outcome. We say in medicine first do no harm but in trying to improve the situation by excising neuroma in continuity or frank neuroma it is a further injury to the nerves. By cutting all the nerves some will never recover from this second ‘injury’ to regrow; After excising the neuroma all the axons have to start growing from this point and any function that was present in that root would be lost until it regrows over months. We thus have to be sure that in doing this we are likely to end up with a better outcome than if we had done a less invasive procedure or no surgery at all. That is why we try to take all the information we can before considering surgery.
When we think the evidence from at least two outpatient clinical assessments and the neurophysiology points towards surgery being able to improve upon what would happen if we didn’t operate (the natural history) then we offer you the parents that option.
The surgery is called fully:
Supraclavicular exploration neurolysis and neurophysiologic assessment (SENNA) +/- Proceed to nerve graft +/- nerve transfers.
The operation is firstly a further and the most thorough assessment of the nerve injury possible plus the opportunity to the reconstruct the nerve injury if that is though necessary. This means we would, (after a further pre operative clinical examination on the ward) ,under general anaesthesia do an operation on the nerves in the neck to free them from scar tissue (the other tissues around the nerves are damaged too and often pinch the nerves). We then do the same neurophysiologic tests that we did before the operation but actually on the nerves directly. Now we have seen and felt the nerves and freed them from scar. At this point we can find that we reclassify the nerve injury as not likely to benefit from the further stage of cutting out the damaged area of nerve. This is a big step to take to decide not to excise the neuroma but if it is the correct decision when all the information is taken in consideration then that is what we do. In some cases we think it necessary just to do a nerve transfer operation instead (which is a lesser intervention) and others both nerve grafting and nerve transfers.
Saying all of this we do know that primary nerve surgery is essential in the most severe cases, many of the other lesser degrees of injury recover well but not perfectly (but importantly would not improve any more if we had undertaken surgery). The key factor in OBPP is shoulder innervation. The C5 root innervates the shoulder and scapula and is the most severlely injured nerve root. Thus our focus in trying to gain the best function we can from any given injury has to have the shoulder at the very centre of this. Elbow function, forearm and hand are of course essential too but these are almost always much less injured than the C5 (shoulder) nerve root.
It is important to realise the complexity of nerve function – nerves don’t just serve movement and feeling; They control growth, development of the bones and joints and muscles, the balance of muscles against each other, the control of movement, the function of skin, the sense of where your body is in space, pain, etc etc etc. Thus the injury to the nerves sustained at birth affects the arm for the rest of growth (and i suppose after that too). The ‘echo’ of the injury is that the imbalance of all these functions of the nerves can create secondary problems right up until growth stops at around 12-16 in girls and 14-18 in boys. The imbalance in muscles around the shoulder leads to shoulder dysplasia (see below – shoulder surgery in OBPP)
Shoulder surgery in OBPP
The most common problem in OBPP is one that affects the shoulder; The nerve injury in OBPP affects the different nerve roots to different extents. This leaves the most severe injury at C5 (at the top of the plexus) and at each lower root in turn a lesser injury. This pattern of injury means that the major concern in recovery is the C5 which relates clinically to shoulder function. The C5 root powers shoulder external rotation (turning the arm out from the side)where as internal rotation (turing the arm back to the abdomen) is powered by C6 and C7 (perhaps even some C8 fibres). This imbalance in injury leads to in imbalance in recovery very common where the power of internal rotation is much greater than its opposite force. It it true of growing tissue that imbalance leads to deformity, just like a sapling growing in a prevailing wind will not grow straight. Thus is created the Obligate internal rotation pathology and the subsequent series of events that leads to gleno-humeral subluxation and then full dislocation.